BY: SAMANTHA BARTLETT, DVM
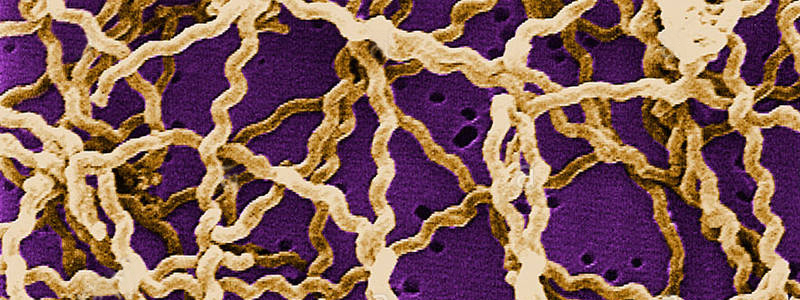
Leptospirosis is a disease state caused by aerobic, gram-negative spirochetes. Leptospirosis in a One Health issue and is the source of widespread global zoonosis. Leptospira bacteria can infect many different mammals and is often transmitted from the environment across mucosal membranes and broken skin. Dogs are more at risk than cats. Transmission to dogs most commonly occurs through contact with wildlife such as raccoons, deer, skunks and rodents or contaminated water sources. While common in the tropics, the bacteria can be found in temperate climates where it tends to be more seasonal in nature.
Of concern has been the increased number of incidences of leptospirosis in dogs in the United States. Traditionally dogs in the at-risk group were outdoor dogs, particularly hunting dogs, in warm, moist climates. New evidence suggests that dogs with no known exposure have tested positive for Leptospira. These dogs include small breed house dogs that only roam outdoors within the confines of a fenced backyard. Just this summer, several dogs were diagnosed with leptospirosis after attending a dog park in California. More than 50 dogs have been diagnosed in Arizona earlier this year. Other areas of higher incidence include New Jersey, Illinois, and Massachusetts.
The movement of suburbs into previously uninhabited areas may have contributed to increased exposure to dogs from wildlife – notably raccoons and skunks. Another contributing factor for the spread of leptospirosis incidence is climate change leading to increased temperatures and flooding. The increased number of dogs traveling and attending “social” events also has had an impact on the spread of disease. Finally, the increased awareness and testing for the disease has contributed to the larger number of reported cases.
The clinical signs vary widely. Most dogs present for flu-like symptoms such as lethargy, inappetance, and fever. Other dogs present with signs of liver failure or renal disease. Testing for suspected leptospirosis cases should be a combination of PCR and antibody testing. Because of the wait time for PCR, any suspected leptospirosis case should be treated as such and hospital staff should use extreme caution when handling these patients, both for their own safety and the safety of other patients.
The CDC has published guidelines for the protection of pets and people from leptospirosis. These include rodent control and vaccination. The CDC also encourages owners to have their pet examined immediately if they suspect Leptospira contamination and to use caution when handling animal tissues and body fluids.
Leptospirosis is not a core vaccine. Traditionally the vaccine was only given to dogs considered at-risk – hunting and working dogs in endemic areas. However, many veterinarians are starting to routinely vaccinate against Leptospirosis regardless of the pet’s perceived lifestyle risks. Most vaccines are protective against multiple serovars and are labeled to protect for 12 months after an initial two vaccine booster period. Many clients are resistant to the idea of vaccinating for Leptospirosis because of the risk of vaccine reactions. Newer vaccines have shown to be no more reactive than other vaccines. The difficulty of diagnosis coupled with the range of clinical signs and zoonotic potential, may make prevention a better course.